Would you run a marathon without water or food?
Climb a mountain?
Have a baby?
Women giving birth expend a tremendous amount of energy. They sweat, urinate, defecate, and generally lose bodily fluids of all kinds.
Against the hospital policy
Yet many hospitals in America continue to restrict what a laboring woman can eat or drink, telling women that eating and drinking during labor is forbidden.
“It’s against hospital policy,” a laboring woman is told.
The idea that eating and drinking during labor is dangerous is a holdover from the late 1940s when Dr. Curtis Mendelson, a New York obstetrician, posited that food could be vomited and then aspirated into the lungs if a patient was under general anesthesia.
Today the relevance of Mendelson’s findings, mostly done on experiments with rabbits, is disputed.
And the fact is that the vast majority of pregnant women, even those who end up delivering via Cesarean section, will not be under general anesthesia.
Cochrane review finds NO benefit to restricting eating and drinking during labor
A systematic review of the scientific literature, published by the Cochrane Institute in 2009, found no benefit to restricting eating and drinking during labor.
Cochrane, a nonprofit independent network of researchers, professionals, caregivers, and patients, gathers and summarizes the best existing scientific evidence to help patients make informed, educated choices. Their reviews are often considered the gold standard of what we know and what we don’t about best practices in medicine.
ACOG has it wrong
But despite the Cochrane findings that there is no benefit to restricting eating and drinking during labor, the American College of Obstetricians and Gynecologists (ACOG), continues to recommend restricting food.
“Allowing laboring women more than a plastic cup of ice is going to be welcome news for many,” William H. Barth, Jr, MD, of Massachusetts General Hospital in Boston and chair of ACOG’s Committee on Obstetric Practice, is reported as saying in a press release about ACOG’s updated guidelines. “As for the continued restriction on food, the reality is that eating is the last thing most women are going to want to do since nausea and vomiting during labor is quite common.”
Eating is the last thing a pregnant woman is going to want to do?
Ah, Dr. Barth, one sees that you have never been in labor or given birth to a baby.
Yes, women sometimes vomit.
Yes, they sometimes feel nauseous.
But they also feel hungry. Sometimes tremendously hungry. I was hungry during my labors.
Especially when a labor lasts a long time, women need to eat and drink.
A woman’s body knows what it needs. You, the laboring women, should be the judge of whether eating and drinking during labor is right. Not your doctor. Or an ACOG guideline.
Having a baby in Norway
If you have a baby in a hospital in Norway, the doctors won’t restrict your food intake.
At the Ullevål Delivery Department at the Oslo University Hospital in Norway, which I visited twice this September, the obstetricians or the midwives (midwives oversee 70 percent of the births in Norway) may even send you downstairs to the cafeteria to get something nourishing to eat.
If you don’t have the energy to walk that far, they have snacks on hand.
In a window-lined room for laboring women and their families in the ABC (Alternative Birth Center) at Ullevål, which has a kitchen, table and chairs, toaster, and microwave, there’s a nice big refrigerator.
Tubs of liver paste, tubes of caviar, butter, fruit juice, and frozen whole grain bread are available to anyone. The laboring woman, the eager spouse, or even the hungry journalist can partake.

Food for laboring women is not discouraged at the hospital in Norway, it is actually provided
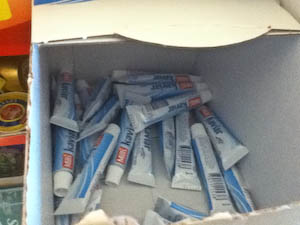
Caviar is a popular food in Norway, available for free on the labor ward to anyone’s who’s hungry
Ironically, in countries that have the best birth practices (and the best maternal and fetal outcomes), their evidence-based practices often come from studies done in the United States.
In Iceland a baby is not washed after birth. Several scientific studies have shown that washing a newborn does more harm than good. In fact, the fluids on a baby’s body are actually good for her skin.
In addition, continuous fetal monitoring is not used during low-risk pregnancies. Why not? Because studies have shown that this kind of monitoring only leads to more unnecessary C-sections and other interventions, not to better outcomes.
And laboring women are allowed to eat and drink what they want when they want it.
In Scandinavian countries eating and drinking during labor is the woman’s choice
Maybe it’s naive. Or maybe it’s clairvoyant. But I like to imagine that one day our birth system will be more like Scandinavia’s.
In addition, I look forward to the day when American doctors will start paying attention to the science and best evidence.
A woman deserves to feel empowered during birth, treated with dignity, and given as much or as little as she wants to eat and drink.
It’s hard work to give birth to a baby. We must treat laboring moms with kindness and respect.
If the hospital where you want to give birth does not “allow” eating and drinking during labor, find a different hospital.
Or, better yet, have your baby at home.
Related articles:
Epidural Alternatives
When You Go Into Labor at Night
Is Tylenol Safe During Pregnancy?
Published: September 27, 2011
Last update: April 27, 2021
As it should be! It’s about time these things start changing in North America… good grief 🙁
Wasn’t at all hungry during my (brief) labor, so this never occurred to me. But for all those women who endure those long labors am sure it’s an issue.
Chalk up one more reason why the case can be made that American obstetricians should not be permitted anywhere near a laboring woman. Far too many c-sections, episiotomies doing the exact opposite of what obstetricians thought they were doing, cutting the cord before it stops pulsating, removing half of the normal skin from the normal penis of a newborn healthy boy, and preventing women from getting empowerment from their births are among the reasons. We must bring humans into the world better if they are to evolve into the type of people who can live sustainably, and possibly keep us from extinction.
The worst part about my 36-hour labor-turned-c-section-turned-3-days-on-clear-liquids was how HUNGRY I was. Okay, that was totally not the worst part. There were WAY worse parts. But it was really dispiriting. I would have given my eye teeth for a ham and cheese croissant while I was laboring away.
I was surprised that I did not want to eat while in labor. I’m the type of person that’s hungry all the time, and I assumed that I would want to eat during labor. My hospital does not have a policy against eating and drinking, but they certainly don’t have tubes of caviar in the fridge. I threw up a number of times during labor with my first child, so I actively avoided food when I was in labor with my second. I still threw up, but it wasn’t as bad. After I’d given birth, however, I was starving. I managed to get food twice each time directly after delivery. I’d get one meal in labor and delivery, and another meal up in postpartum. My hospital, by the time I had my second, also changed how patient meals were served. I could order as much as I wanted from a very large menu. And I did! Ultimately, it’s important for hospitals to support a woman’s decision about what she wants to eat and drink and when.
Thank you for posting this. THIRST was what overcame me during my first labor, which was a very dehydrating 36 hours long. Even though I had IV fluids, I was so desperately thirsty I had trouble concentrating on birthing. I begged for a cup of water, and was given only a few ice chips by the nurse. It was horrible and I felt abused to be denied a drink of water for so long. The baby wasn’t coming down and when I could stand it no longer, I screamed for my husband to give me water and he grabbed his cup and gave it to me. Then I could finally concentrate, and minutes later I delivered my baby boy.